The standard recommendation for anyone experiencing anaphylaxis is: administer epinephrine promptly in the reaction, and call 9-1-1 to have an ambulance take you to the emergency department.
But with the coronavirus pandemic, the trouble is, no one wants to go to the emergency department and risk exposure to the new virus. A common question allergists and food allergy non-profits are hearing is: At this time, do we have to call 9-1-1 after administering epinephrine?
Now Dr. Thomas Casale, an allergist and chief medical adviser for operations of the non-profit FARE (Food Allergy Research and Education), and two colleagues address the question. In a paper published the week of April 20, they offer a modified anaphylaxis emergency care plan for allergists to consider recommending to patients and families.
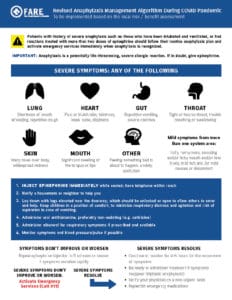
Especially in areas where emergency departments remain overwhelmed by the COVID-19 crisis, Casale says that while “an anaphylactic event is very serious, at-home care is possible in many situations so long as extra precautions are taken on behalf of both patients and caregivers.” The revised emergency care plan (called a management algorithm) starts by stating that “it is critical for patients to have at least two epinephrine auto-injectors available for management.”
It offers guidance for at-home treatment and monitoring of food-allergic reactions. There are key exceptions: with a history of severe reactions or anaphylaxis that’s not resolving, the authors advise calling 9-1-1 without hesitation.
What the Revised Plan Says
Under the revised emergency care plan, allergists would advise parents and adult patients to:
• Administer an auto-injector immediately for symptoms of a severe allergic reaction.
• After that, take an antihistamine (such as cetirizine), or use prescribed albuterol for respiratory symptoms.
• Monitor the patient’s response to see whether severe symptoms resolve promptly (such as wheezing, shortness of breath or difficulty breathing, faintness, low blood pressure, vomiting, throat swelling).
• If severe symptoms don’t resolve within about 5 minutes or they worsen, administer a second dose of epinephrine.
• If after the second dose of epinephrine, severe symptoms are not resolving, call 911 to get immediate medical assistance.
• If the symptoms do resolve promptly, continue to monitor for 4-6 hours. Be ready to inject another epinephrine dose in case of a secondary reaction (called a biphasic reaction).
• With symptoms that resolved, inform your doctor of the reaction on a non-urgent basis. Be sure to replenish your supply of epinephrine and/or other medications.
Interview with Dr. Casale
Allergic Living editor Gwen Smith spoke to Dr. Thomas Casale about the revised anaphylaxis emergency protocol that he is recommending, along with his allergist co-authors Dr. Julie Wang (Mount Sinai school of medicine) and Dr. Anna Nowak-Wegrzyn (NYU Langone).
What is the main reason for this new advice?
Dr. Thomas Casale: I think it’s the reluctance now to go to the emergency department and possibly be exposed to someone who has COVID-19. That will vary by region. If you’re in New York City, that’s a much different scenario than perhaps in a rural community in a state like Wyoming.
Following a second dose of epinephrine, if you or your child is still having severe symptoms, your plan says to “activate emergency services.” Is that calling 9-1-1, which is overburdened in some places, or is it alright to drive to a close hospital?
TC: It’s a good question, and it’s going to depend upon where you’re located. Certainly, we prefer people calling 9-1-1 because, if the ambulance gets there in a in a timely fashion, they have access to adrenaline, they can intubate somebody, they could start IVs. That would be the preferred route.
However, if you’re in an area where you know the [emergency services] response times are very long and you’re relatively close to a hospital, it’s going to be a judgment call. This should be considered in conjunction with the patient’s own physician. We don’t want them to decide this on their own, but to talk with their physician to see if this [revised plan] makes sense for them.
In the revised plan, you say to administer an oral antihistamine after giving epinephrine. And you mention using an albuterol inhaler, if prescribed for asthma. Those steps won’t be in all current emergency plans. Are you and your co-authors being more proactive at a time when patients are less likely to go to the ED?
TC: It is being a little bit more proactive. When we treat anaphylaxis, epinephrine is the go-to drug and we’re just saying if you do have an antihistamine, which I assume that most people would have – they could take an oral antihistamine after they inject the epinephrine. But we do not want them to stall in the use of epinephrine by taking the antihistamine first.
Having that antihistamine on board might reduce the magnitude of that reaction. It’s probably not going to protect you completely, but it might help a bit to reduce the magnitude of the reaction.
And it’s the same with administering albuterol, if they have lower respiratory symptoms. If the patient has asthma, they may have wheezing with an anaphylactic event. So they should use their albuterol as well. But again, epinephrine should be the first drug in anaphylaxis.
This paper puts emphasis on contacting your allergist and anaphylaxis management planning during the pandemic. This is stressed especially with a history of severe anaphylaxis.
TC: Yes, I think now is the time when you want to have this discussion with your allergist. Is this new algorithm appropriate for me? What are the types of medications I should have available?
We know that everybody [with food and sting allergies] should have have two epinephrine auto-injectors. But if you’re a patient with a history of biphasic reactions or more severe reactions, do you have more than two? Should you have three or four? When do you seek emergency care vs. trying to work through this algorithm? So those types of discussions should be done.
If you’re a patient who has had to use epinephrine in the past for severe reaction, then for sure we would want you to consult with your physician as to whether this algorithm is OK for you to try. Or whether you should just stick with what your allergist advised you previously.
Do people actually face a heightened risk of COVID-19 exposure at the emergency department? Hospitals do have protocols.
TC: Yes, ICUs [intensive care units] are being separated into COVID-19 vs. non-COVID-19 in-patient units. In the ED, that’s the same, people are being separated.
However, you would be in contact with other people who could be infected and asymptomatic, including everyone from the paramedic to the person who checks you into the emergency room. They are wearing personal protection equipment, but it’s something to consider.
If you’re in a city or town where hospitals are not overwhelmed by coronavirus, would you still follow the newer plan, or would you go with the standard advice to use epinephrine and call 9-1-1?
TC: This is a good discussion to have with your allergist as to whether you should use this [plan] or not. The other piece of it is your own comfort level. Is it very anxiety-provoking for you to go to the emergency room or go into an ambulance during this time? These are things that you have to weigh and discuss with your allergist to make the correct decision in the location where you live and for the individual who has the allergies.
History of Severe Anaphylaxis: The graphic of the revised emergency plan (shown above) notes boldly that an exception in the advice to treat with epinephrine and monitor would be patients with history of severe anaphylaxis, “such as those who have been intubated and ventilated, or had reactions treated with more than two doses of epinephrine.” They are advised to follow their routine anaphylaxis plan and call 9-1-1 immediately when anaphylaxis is recognized.
This new advice about when to visit the emergency department is also in keeping with guidelines published in March 2020 for allergists’ offices during the pandemic. They suggest that allergists suspend “the routine advice on allergy action plans to seek emergency care/call 911 after epinephrine use, unless symptoms do not immediately resolve without recurrence after a single dose of epinephrine.”
Both papers were published in The Journal of Allergy and Clinical Immunology: In Practice.
Related Reading:
Acute At Home Management of Anaphylaxis During the COVID-19 Pandemic
FARE’s News Release About the Revised Emergency Care Plan
Allergic Living’s COVID-19 and Allergies, Asthma Hub
All About Epinephrine Guide